“Diabetes mellitus” refers to a group of diseases which affect the way your body uses your blood sugar (glucose). The importance of Glucose in your health is due to that fact that it's an important source of energy for the cells that make up your muscles and tissues. It's also your brain's main source of fuel.
The underlying cause of diabetes varies by the type it falls under. But, no matter what type of diabetes you have, it can lead to excess sugar in your blood. Too much sugar in your blood can lead to serious health problems.
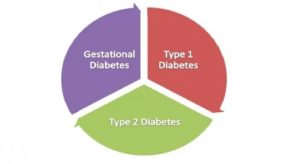 Types of Diabetes
Types of Diabetes
Chronic diabetes conditions include type 1 diabetes and type 2 diabetes. Potentially reversible diabetes conditions include prediabetes — when your blood sugar levels are higher than normal, but not high enough to be classified as diabetes — and gestational diabetes, which occur only during pregnancy but may resolve after the baby is delivered.
Symptoms
The symptoms of Diabetes can vary depending on how much your blood sugar is elevated. Some people, especially those with prediabetes or type 2 diabetes, may not experience symptoms initially. In type 1 diabetes, symptoms tend to come on quickly and be more severe.
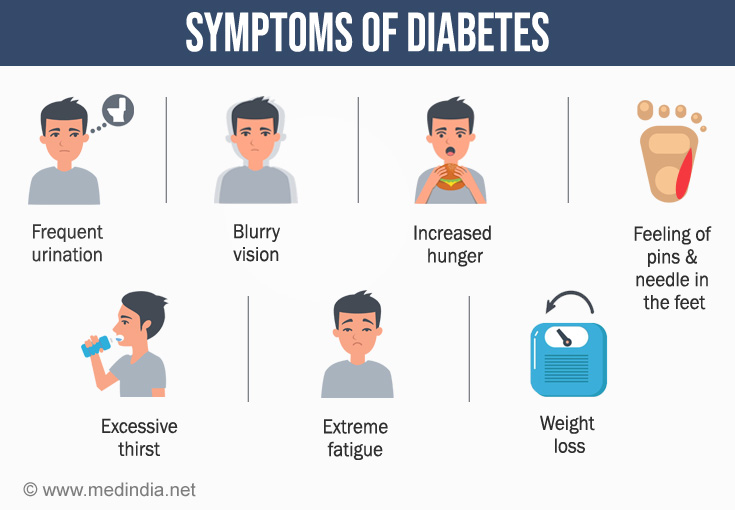
- Increased thirst
- Frequent urination
- Extreme hunger
- Unexplained weight loss
- Presence of ketones in the urine (ketones are a byproduct of the breakdown of muscle and fat that happens when there's not enough available insulin)
- Fatigue
- Irritability
- Blurred vision
- Slow-healing sores
- Frequent infections, such as gums or skin infections and vaginal infections
Type 1 diabetes can strike anyone, from any walk of life. It can develop at any age, though it often appears during childhood or adolescence. Type 2 diabetes, the more common type, can develop at any age, though it's more common in people older than 40.
In the last decade, the cases of people living with diabetes jumped almost 50 percent – to more than 30 million Americans. Worldwide, it afflicts more than 422 million people. Diabetes is a leading cause of blindness, kidney failure, amputations, heart failure, and stroke.
Diagnosis

Symptoms of type 1 diabetes often appear suddenly and are often the reason for checking blood sugar levels. Because symptoms of other types of diabetes and prediabetes come on more gradually or may not be evident, the American Diabetes Association (ADA) has recommended screening guidelines. The ADA recommends that the following people be screened for diabetes:
- Anyone with a body mass index higher than 25 (23 for Asian-Americans), regardless of age, who has additional risk factors, such as high blood pressure, abnormal cholesterol levels, a sedentary lifestyle, a history of polycystic ovary syndrome or heart disease, and having a close relative with diabetes.
- Anyone older than age 45 is advised to receive an initial blood sugar screening, and then, if the results are normal, to be screened every three years thereafter.
- Any woman who has had gestational diabetes is advised to be screened for diabetes every three years.
- Anyone who has been diagnosed with prediabetes is advised to be tested every year.
Tests for type 1 and type 2 diabetes and prediabetes
- Glycated hemoglobin (A1C) test. This blood test, which doesn't require fasting, indicates your average blood sugar level for the past two to three months. It measures the percentage of blood sugar attached to hemoglobin, the oxygen-carrying protein in red blood cells.
- The higher your blood sugar levels, the more hemoglobin you'll have with sugar attached. An A1C level of 6.5 percent or higher on two separate tests indicates that you have diabetes. An A1C between 5.7 and 6.4 percent indicates prediabetes. Below 5.7 is considered normal.
- Random blood sugar test. A blood sample will be taken at a random time. Regardless of when you last ate, a random blood sugar level of 200 milligrams per deciliter (mg/dL) — 11.1 millimoles per liter (mmol/L) — or higher suggests diabetes.
- Fasting blood sugar test. A blood sample will be taken after an overnight fast. A fasting blood sugar level less than 100 mg/dL (5.6 mmol/L) is normal. A fasting blood sugar level from 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is considered prediabetes. If it's 126 mg/dL (7 mmol/L) or higher on two separate tests, you have diabetes.
- Oral glucose tolerance test. For this test, you fast overnight, and the fasting blood sugar level is measured. Then you drink a sugary liquid, and blood sugar levels are tested periodically for the next two hours.
- A blood sugar level less than 140 mg/dL (7.8 mmol/L) is normal. A reading of more than 200 mg/dL (11.1 mmol/L) after two hours indicates diabetes. A reading between 140 and 199 mg/dL (7.8 mmol/L and 11.0 mmol/L) indicates prediabetes.
If type 1 diabetes is suspected, your urine will be tested to look for the presence of a byproduct produced when muscle and fat tissue are used for energy because the body doesn't have enough insulin to use the available glucose (ketones). Your doctor will also likely run a test to see if you have the destructive immune system cells associated with type 1 diabetes called autoantibodies.
Tests for gestational diabetes

Your doctor will likely evaluate your risk factors for gestational diabetes early in your pregnancy:
- If you're at high risk of gestational diabetes — for example, if you were obese at the start of your pregnancy; you had gestational diabetes during a previous pregnancy; or you have a mother, father, sibling or child with diabetes — your doctor may test for diabetes at your first prenatal visit.
- If you're at average risk of gestational diabetes, you'll likely have a screening test for gestational diabetes sometime during your second trimester — typically between 24 and 28 weeks of pregnancy.
- Initial glucose challenge test. You'll begin the glucose challenge test by drinking a syrupy glucose solution. One hour later, you'll have a blood test to measure your blood sugar level. A blood sugar level below 140 mg/dL (7.8 mmol/L) is usually considered normal on a glucose challenge test, although this may vary at specific clinics or labs. If your blood sugar level is higher than normal, it only means you have a higher risk of gestational diabetes. Your doctor will order a follow-up test to determine if you have gestational diabetes.
- Follow-up glucose tolerance testing. For the follow-up test, you'll be asked to fast overnight and then have your fasting blood sugar level measured. Then you'll drink another sweet solution — this one containing a higher concentration of glucose — and your blood sugar level will be checked every hour for a period of three hours. If at least two of the blood sugar readings are higher than the normal values established for each of the three hours of the test, you'll be diagnosed with gestational diabetes
Managing Diabetes
 Depending on what type of diabetes you have, blood sugar monitoring, insulin, and oral medications may play a role in your treatment. Eating a healthy diet, maintaining a healthy weight and participating in regular activity also are important factors in managing diabetes.
Depending on what type of diabetes you have, blood sugar monitoring, insulin, and oral medications may play a role in your treatment. Eating a healthy diet, maintaining a healthy weight and participating in regular activity also are important factors in managing diabetes.
Treatments for all types of diabetes
An important part of managing diabetes — as well as your overall health — is maintaining a healthy weight through a healthy diet and exercise plan:
- Healthy eating - Understanding what and how much to eat can be a challenge. A registered dietitian can help you create a meal plan that fits your health goals, food preferences, and lifestyle. This will likely include carbohydrate counting, especially if you have type 1 diabetes.
- Engage in Physical activity- Aim for at least 30 minutes or more of aerobic exercise most days of the week. Bouts of activity can be as brief as 10 minutes, three times a day. If you haven't been active for a while, start slowly and build up gradually.

Treatment for type 1 diabetes involves insulin injections or the use of an insulin pump, frequent blood sugar checks, and carbohydrate counting. Treatment of type 2 diabetes primarily involves lifestyle changes, monitoring of your blood sugar, along with diabetes medications, insulin or both.
Monitoring your blood sugar- Depending on your treatment plan, you may check and record your blood sugar as many as four times a day or more often if you're taking insulin. Careful monitoring is the only way to make sure that your blood sugar level remains within your target range. People with type 2 diabetes who aren't taking insulin generally check their blood sugar much less frequently.
- People who receive insulin therapy also may choose to monitor their blood sugar levels with a continuous glucose monitor. Although this technology hasn't yet completely replaced the glucose meter, it can significantly reduce the number of fingersticks necessary to check blood sugar and provide important information about trends in blood sugar levels.
- Even with careful management, blood sugar levels can sometimes change unpredictably. With help from your diabetes treatment team, you'll learn how your blood sugar level changes in response to food, physical activity, medications, illness, alcohol, stress — and for women, fluctuations in hormone levels.
- In addition to daily blood sugar monitoring, your doctor will likely recommend regular A1C testing to measure your average blood sugar level for the past two to three months.
- Compared with repeated daily blood sugar tests, A1C testing better indicates how well your diabetes treatment plan is working overall. An elevated A1C level may signal the need for a change in your oral medication, insulin regimen or meal plan.
- Your target A1C goal may vary depending on your age and various other factors, such as other medical conditions you may have. However, for most people with diabetes, the American Diabetes Association recommends an A1C of below 7 percent. Ask your doctor what your A1C target is.
- People with type 1 diabetes need insulin therapy to survive. Many people with type 2 diabetes or gestational diabetes also need insulin therapy.
- Many types of insulin are available, including rapid-acting insulin, long-acting insulin, and intermediate options. Depending on your needs, your doctor may prescribe a mixture of insulin types to use throughout the day and night.
- Insulin can't be taken orally to lower blood sugar because stomach enzymes interfere with insulin's action. Often insulin is injected using a fine needle and syringe or an insulin pen — a device that looks like a large ink pen.
- An insulin pump also may be an option. The pump is a device about the size of a cellphone worn on the outside of your body. A tube connects the reservoir of insulin to a catheter that's inserted under the skin of your abdomen.
- A tubeless pump that works wirelessly also is now available. You program an insulin pump to dispense specific amounts of insulin. It can be adjusted to deliver more or less insulin depending on meals, activity level and blood sugar level.
- An emerging treatment approach, not yet available, is closed-loop insulin delivery, also known as the artificial pancreas. It links a continuous glucose monitor to an insulin pump and automatically delivers the correct amount of insulin when needed.
- There are a number of versions of the artificial pancreas, and clinical trials have had encouraging results. More research needs to be done before a fully functional artificial pancreas receives regulatory approval.
- However, progress has been made toward an artificial pancreas. In 2016, an insulin pump combined with a continuous glucose monitor and a computer algorithm was approved by the Food and Drug Administration. However, the user still needs to tell the machine how many carbohydrates will be eaten.
- Sometimes other oral or injected medications are prescribed as well. Some diabetes medications stimulate your pancreas to produce and release more insulin. Others inhibit the production and release of glucose from your liver, which means you need less insulin to transport sugar into your cells.
- Still, others block the action of the stomach or intestinal enzymes that break down carbohydrates or make your tissues more sensitive to insulin. Metformin (Glucophage, Glumetza, others) is generally the first medication prescribed for type 2 diabetes.
- In some people who have type 1 diabetes, a pancreas transplant may be an option. Islet transplants are being studied as well. With a successful pancreas transplant, you would no longer need insulin therapy.
- But transplants aren't always successful — and these procedures pose serious risks. You need a lifetime of immune-suppressing drugs to prevent organ rejection. These drugs can have serious side effects, which is why transplants are usually reserved for people whose diabetes can't be controlled or those who also need a kidney transplant.
Although it is not specifically considered a treatment for type 2 diabetes, people with type 2 diabetes who are obese and have a body mass index higher than 35 may benefit from this type of surgery. People who've undergone gastric bypass have seen significant improvements in their blood sugar levels. However, this procedure's long-term risks and benefits for type 2 diabetes aren't yet known.
Treatment for gestational diabetes
Controlling your blood sugar level is essential to keeping your baby healthy and avoiding complications during delivery. In addition to maintaining a healthy diet and exercising, your treatment plan may include monitoring your blood sugar and, in some cases, using insulin or oral medications.
Your doctor also will monitor your blood sugar level during labor. If your blood sugar rises, your baby may release high levels of insulin — which can lead to low blood sugar right after birth.
Treatment for prediabetes

If you have prediabetes, healthy lifestyle choices can help you bring your blood sugar level back to normal or at least keep it from rising toward the levels seen in type 2 diabetes. Maintaining a healthy weight through exercise and healthy eating can help. Exercising at least 150 minutes a week and losing about 7 percent of your body weight may prevent or delay type 2 diabetes.
Sometimes medications — such as metformin (Glucophage, Glumetza, others) — also are an option if you're at high risk of diabetes, including when your prediabetes is worsening or if you have cardiovascular disease, fatty liver disease or polycystic ovary syndrome.
In other cases, medications to control cholesterol — statins, in particular — and high blood pressure medications are needed. Your doctor might prescribe low-dose aspirin therapy to help prevent cardiovascular disease if you're at high risk. However, healthy lifestyle choices remain key.
Ongoing & Future Trends in Treating Diabetes
Cell therapy for Type-1- Diabetes:
Although still in the very early stages of development, cell therapy is one of the biggest hopes of developing a cure for diabetes, especially for type 1 diabetes. Replacing the missing insulin-producing cells has the potential to recover normal insulin production and cure patients.
However, early attempts at the transplantation of pancreatic cells have largely failed, mostly due to immune reactions against donor cells that cause complications and eventually destroy the implanted cells. The lack of donors is also a limitation. One of the most advanced alternatives comes from the Diabetes Research Institute (DRI) in the US, which is developing a bioengineered mini-organ where insulin-producing cells are encapsulated within a protective barrier. Two years ago, the DRI announced that the first patient treated in an ongoing Phase I/II trial no longer requires insulin therapy.
A vaccine for diabetes:A vaccine for type 1 diabetes that could transform the lives of those at high risk of the condition could be a reality within the next 20 years, according to Dr Alasdair Rankin, Diabetes UK’s Director of Research. This would represent the biggest single breakthrough in diabetes research since insulin was first successfully used to treat type 1 diabetes 91 years ago.
A device that Improves the engraftment of insulin-producing cells:The beginning of a new era in islet transplantation. The ultimate goal of Diabetes research institute’s device is to prevent the need for life-long anti-rejection therapy. Another similar device is being developed by Viacyte, in collaboration with the Juvenile Diabetes Research Foundation (JDRF) in the UK. After a Phase I trial where the device proved safe, the company is now working on improving the engraftment of insulin-producing cells.
Beta cell replacement therapy :Big pharma is in the early stages of developing their own cell therapy approaches for diabetes. Novo Nordisk, one of the largest providers of diabetes treatments, is bidding for stem cells and an encapsulation device, stating that the first clinical trial could take place in the “next few years.” Sanofi, also a big name in diabetes, is working with the German Evotec in a beta cell replacement therapy for diabetics.
New injection to control blood sugar:A new once a day injectable treatment was approved by the European Medicines Agency in 2013. According to recent reports in the Herald Scotland, Lyxumia is a treatment for adults with type 2 diabetes and is taken in combination with other glucose-controlling drugs, together with diet and exercise, where these alone have not controlled adequate glycaemic control.
Gene therapy:New research by Dr Alexey Pshezhetsky of the Sainte-Justine University Hospital Research Center in Canada, published this year has discovered insulin resistance in type 2 diabetes is caused partly by a lack of a protein – a breakthrough that may help develop a treatment to prevent the disease. The protein, Neu1, turns the absorption of sugar "on" or "off" in body cells, by regulating the amount of sialic acid on the surface of cells. Scientists are now trying to find a way to restore Neu1 levels and function in diabetes to force the insulin receptor to do its job of absorbing blood sugar properly.
Countering the immune systemActoBio Therapeutics, in Belgium, is about to start another clinical trial with an unusual approach to stop type 1 diabetes. The company uses cheese-producing bacteria to deliver two drugs that stimulate regulatory T cells to instruct the immune system not to attack insulin-producing cells.
Also getting close to the clinic is Neovacs, developing a vaccine for type 1 diabetes intended to delay the progression of type 1 diabetes after early diagnosis. The treatment is focused on lowering the levels of an inflammatory protein that is thought to be involved in multiple autoimmune diseases, including type 1 diabetes but also lupus.
The artificial pancreasEfforts to cure or stop type 1 diabetes are still in the early stages, and these approaches will also not be suitable for people that have already lost their insulin-producing cells. A solution could be the creation of an “artificial pancreas” — a fully automated system that can measure glucose levels and inject the right amount of insulin into the bloodstream, just like a healthy pancreas would.
Inducing insulin productionOne of the biggest hits in type 2 diabetes treatment is a glucagon-like peptide (GLP)-1 receptor agonists, which induce insulin production in beta-pancreatic cells while suppressing the secretion of glucagon. All big pharma have GLP-1 drugs on the market or their pipelines, including Sanofi, Eli Lilly, Roche, AstraZeneca, and Boehringer Ingelheim. But Novo Nordisk is going a step further with the first oral version of a GLP-1 drug, which is now close to the market.
The French company Poxel is going after a different approach with a drug that simultaneously targets the pancreas, the liver, and the muscles, where it helps recover the lost function of mitochondria, which is thought to drive the progression of type 2 diabetes.
Drug that controls sugar levels & Blood pressure:In Sweden, Betagenon and Baltic Bio are working on a first-in-class drug with the potential to simultaneously control sugar levels and reduce blood pressure, a big risk factor in patients with type 2 diabetes who are also obese. Tackling the obesity component of type 2 diabetes is also the German MorphoSys, which is running Phase II trials with an antibody designed to reduce fat, prevent insulin resistance and control excessive eating.
Sensing acetone in the body- a biomarker associated with blood glucose:Engineers at the University of Michigan in the United States are testing a wearable vapor
- a sensor that can "smell" high blood glucose.
- Research is underway to develop a test that measures blood glucose by analyzing the user's breath.
- Temporary tattoos that monitor blood glucose levels may also be available someday, once developers figure out how to get their readings to the user.
Just in the past decade, scientists have realized the big role that the microbes living inside and on us play in our health. The human microbiome, and especially the gut microbiome, has been found to be linked to multiple chronic diseases, including diabetes. An unbalanced microbiome composition, known as dysbiosis, has been found in patients with diabetes, for whom the diversity of the gut microbiome is often reduced as compared to healthy people. Researchers from the University of Amsterdam recently showed that fecal transplants, used to transfer the microbiome of a healthy person to the gut of one with diabetes, can result in a short-term improvement of the insulin resistance found in obese patients with type 2 diabetes.
Some companies are now starting taking the concept into treatment, with the French Valviotis currently conducting preclinical testing of a drug aimed at increasing the microbiome diversity as a treatment for diabetes. Although promising, the microbiome field is very young and its complexity makes it difficult to establish causation after finding a correlation. Until more diabetes treatments are tested in the clinic, it will be difficult to determine the real potential of the microbiome in this space.
The needle-free revolutionMany companies are trying to develop non-invasive methods to substitute finger pricking. Gal’s company, Integrity Applications, has developed a device called GlucoTrack that can measure glucose using electromagnetic waves and is already available in Europe. Similar technologies are popping up, with GlucoSense in London using laser light to measure sugar levels and MediWise making use of radio waves.
Patches are also becoming a popular form of measuring blood glucose without needles, such as FreeStyle Libre, an inch-wide patch that can be worn for up to 2 weeks. At the University of Bath, researchers are developing a graphene patch that could provide greater accuracy by measuring sugar levels individually in multiple hair follicles.
Others are going for implants, such as NovioSense’s eye implant or Senseonic’s subcutaneous device, which will be distributed by Roche. Still, non-invasive options to measure blood sugar often face issues regarding accuracy. The famous glucose-measuring contact lens that Google announced in 2014 was dismissed as “technically infeasible” and further developments will be needed to reach the degree of accuracy of finger-pricking methods.
Our bodies may cure themselves of diabetes in the futureIn collaboration with other international researchers, researchers at the University of Bergen have discovered that glucagon-producing cells in the pancreas, can change identity and adapt so that they do the job for their neighboring damaged or missing insulin cells. They believe that we are possibly facing the start of a totally new form of treatment for diabetes, where the body can produce its own insulin, with some start-up help
ConclusionThe diabetes market is expected to reach a massively big €86Bn by 2025 combining both type 1 (€32Bn) and type 2 (€54Bn) treatments, and we can expect all sort of revolutionary technologies to come forward and claim their market share. Researchers are already speculating about microchips that can diagnose diabetes type 1 before the symptoms appear or nanorobots traveling in the bloodstream while they measure glucose and deliver insulin.
Whatever the future brings, let's hope that it will undoubtedly make a huge difference in the lives of millions of people worldwide suffering from Diabetes!
Sources:https://www.diabetesresearch.org/what-is-diabetes https://www.mayoclinic.org/diseases-conditions/diabetes/diagnosis-treatment/drc-20371451 https://labiotech.eu/features/diabetes-treatment-cure-review/ https://www.accu-chek.in/more-topics/future-diabetes-treatment https://www.axappphealthcare.co.uk/health-information/diabetes/the-future-of-diabetes-treatments/ https://www.biorasi.com/blog/the-future-of-diabetes-treatment/ https://www.sciencedaily.com/releases/2019/01/190104104020.htm















Leave a Reply