What is a Cardiovascular disease?
Cardiovascular disease is a general term used to describe a range of heart disorders affecting your heart. It can also refer to a wide range of conditions including heart disease, heart attack, stroke, heart failure, Arrhythmia, Heart valve problems, etc.
Heart Disease
Heart and blood vessel disease (also called heart disease) includes numerous problems, many of which are related to a process called atherosclerosis (which is a condition that develops when a substance called plaque builds up in the walls of the arteries). This buildup narrows the arteries, making it harder for blood to flow through. If a blood clot forms, it can block the blood flow. This can cause a heart attack or stroke.
Heart Attack
A heart attack occurs when the blood flow to a part of the heart is blocked by a blood clot. If this clot cuts off the blood flow completely, the part of the heart muscle supplied by that artery begins to die. Most people survive their first heart attack and return to their normal lives, enjoying many more years of productive activity. But experiencing a heart attack does mean that you need to make some serious lifestyle changes. The medications and lifestyle changes that your doctor recommends may vary according to how badly your heart was damaged, and to what degree of heart disease caused the heart attack.
Stroke
An ischemic stroke (the most common type of stroke) occurs when a blood vessel that feeds the brain gets blocked, usually from a blood clot. When the blood supply to a part of your brain is cut off, some brain cells will begin to die. This can result in the loss of functions controlled by that part of the brain, such as walking or talking. A hemorrhagic stroke occurs when a blood vessel within the brain bursts. This is most often caused by uncontrolled hypertension (high blood pressure). Some effects of stroke are permanent if too many brain cells die after being starved of oxygen. These cells are never replaced. The good news is that sometimes brain cells don’t die during the stroke — instead, the damage is temporary. Over time, as injured cells repair themselves, previously impaired function improves. (In other cases, undamaged brain cells nearby may take over for the areas of the brain that were injured.) Either way, strength may return, speech may get better and memory may improve. This recovery process is what stroke rehabilitation is all about.
Heart Failure
Heart failure, sometimes called congestive heart failure, means the heart isn’t pumping blood as well as it should. Heart failure does not mean that the heart stops beating — that’s a common misperception. Instead, the heart keeps working, but the body’s need for blood and oxygen isn’t being met. Heart failure can get worse if left untreated. If your loved one has heart failure, it’s very important to follow the doctor’s orders.
Arrhythmia
Arrhythmia refers to abnormal heart rhythm. There are various types of arrhythmias. The heart can beat too slow, too fast or irregularly. Bradycardia, or a heart rate that’s too slow, is when the heart rate is less than 60 beats per minute. Tachycardia, or a heart rate that’s too fast, refers to a heart rate of more than 100 beats per minute. An arrhythmia can affect how well your heart works. With an irregular heartbeat, your heart may not be able to pump enough blood to meet your body’s needs.
Heart Valve Problems
When heart valves don’t open enough to allow the blood to flow through as it should, a condition called stenosis results. When the heart valves don’t close properly and thus allow blood to leak through, it’s called regurgitation. If the valve leaflets bulge or prolapse back into the upper chamber, it’s a condition called prolapse.
What are the symptoms of Cardiovascular diseases?
Heart disease symptoms depend on what type of heart disease you have.
Symptoms of heart disease in your blood vessels (atherosclerotic disease)
Cardiovascular disease symptoms may be different for men and women. For instance, men are more likely to have chest pain; women are more likely to have other symptoms along with chest discomforts, such as shortness of breath, nausea and extreme fatigue.
Symptoms include:
- Chest pain, chest tightness, chest pressure and chest discomfort (angina)
- Shortness of breath
- Pain, numbness, weakness or coldness in your legs or arms if the blood vessels in those parts of your body are narrowed
- Pain in the neck, jaw, throat, upper abdomen or back
You might not be diagnosed with cardiovascular disease until you have a heart attack, angina, stroke or heart failure. It's important to watch for cardiovascular symptoms and discuss concerns with your doctor. Cardiovascular disease can sometimes be found early with regular evaluations.
Symptoms caused by abnormal heartbeats (heart arrhythmias)
A heart arrhythmia is an abnormal heartbeat. Your heart may beat too quickly, too slowly or irregularly. Heart arrhythmia symptoms can include:
- Fluttering in your chest
- Racing heartbeat (tachycardia)
- Slow heartbeat (bradycardia)
- Chest pain or discomfort
- Shortness of breath
- Lightheadedness
- Dizziness
- Fainting (syncope) or near fainting
Symptoms caused by heart defects
Serious congenital heart defects — defects you're born with — usually become evident soon after birth. Heart defect symptoms in children could include:
- Pale gray or blue skin color (cyanosis)
- Swelling in the legs, abdomen or areas around the eyes
- In an infant, shortness of breath during feedings, leading to poor weight gain
Less serious congenital heart defects are often not diagnosed until later in childhood or during adulthood. Signs and symptoms of congenital heart defects that usually aren't immediately life-threatening include:
- Easily getting short of breath during exercise or activity
- Easily tiring during exercise or activity
- Swelling in the hands, ankles or feet
Symptoms caused by weak heart muscle (dilated cardiomyopathy)
In the early stages of cardiomyopathy, you may have no symptoms. As the condition worsens, symptoms may include:
- Breathlessness with exertion or at rest
- Swelling of the legs, ankles, and feet
- Fatigue
- Irregular heartbeats that feel rapid, pounding or fluttering
- Dizziness, lightheadedness, and fainting
Symptoms caused by heart infections
Endocarditis is an infection that affects the inner membrane that separates the chambers and valves of the heart (endocardium). Heart infection symptoms can include:
- Fever
- Shortness of breath
- Weakness or fatigue
- Swelling in your legs or abdomen
- Changes in your heart rhythm
- Dry or persistent cough
- Skin rashes or unusual spots
Symptoms caused by valvular heart disease
The heart has four valves — the aortic, mitral, pulmonary and tricuspid valves — that open and close to direct blood flow through your heart. Valves may be damaged by a variety of conditions leading to narrowing (stenosis), leaking (regurgitation or insufficiency) or improper closing (prolapse).
Depending on which valve isn't working properly, valvular heart disease symptoms generally include:
- Fatigue
- Shortness of breath
- Irregular heartbeat
- Swollen feet or ankles
- Chest pain
- Fainting (syncope)
What Causes Cardiovascular Diseases?
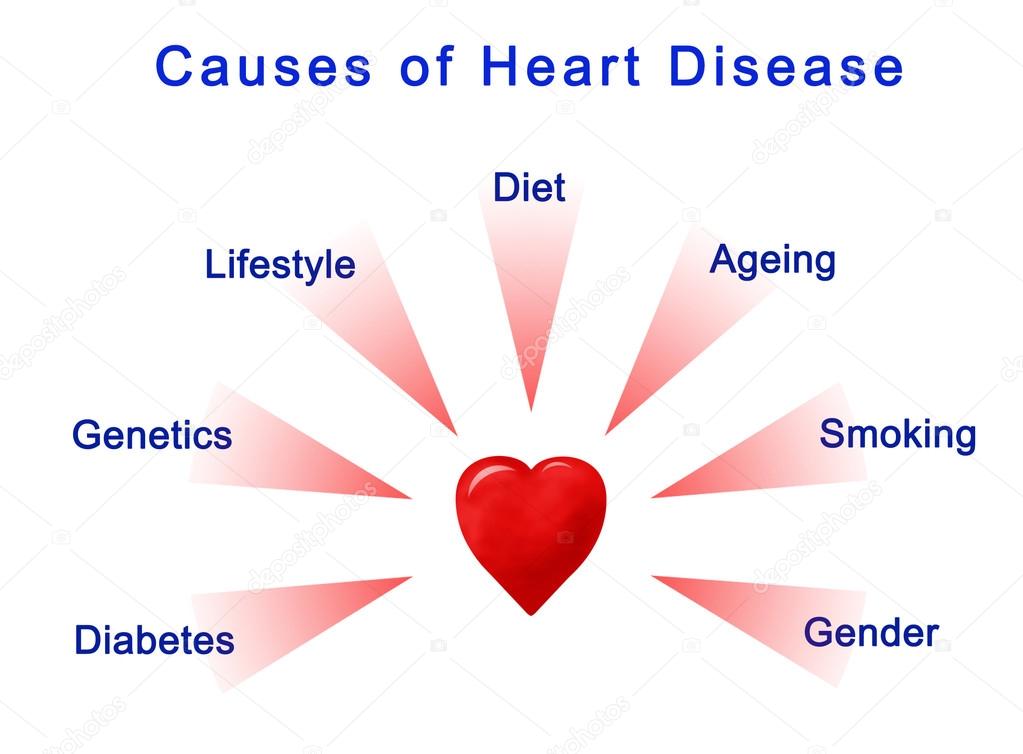
The causes of heart disease vary by its type and they are as follows:
Development of atherosclerosis
While cardiovascular disease can refer to different heart or blood vessel problems, the term is often used to mean damage to your heart or blood vessels by atherosclerosis, a buildup of fatty plaques in your arteries. Plaque buildup thickens and stiffens artery walls, which can inhibit blood flow through your arteries to your organs and tissues. Atherosclerosis is also the most common cause of cardiovascular disease. It can be caused by correctable problems, such as an unhealthy diet, lack of exercise, being overweight and smoking.
Causes of heart arrhythmia
Common causes of abnormal heart rhythms (arrhythmias) or conditions that can lead to arrhythmias include:
- Heart defects you're born with (congenital heart defects)
- Coronary artery disease
- High blood pressure
- Diabetes
- Smoking
- Excessive use of alcohol or caffeine
- Drug abuse
- Stress
- Some over-the-counter medications, prescription medications, dietary supplements, and herbal remedies
- Valvular heart disease
In a healthy person with a normal, healthy heart, it's unlikely for a fatal arrhythmia to develop without some outside trigger, such as an electrical shock or the use of illegal drugs. That's primarily because a healthy person's heart is free from any abnormal conditions that cause an arrhythmia, such as an area of scarred tissue. However, in a heart that's diseased or deformed, the heart's electrical impulses may not properly start or travel through the heart, making arrhythmias more likely to develop.
Causes of congenital heart defects
Congenital heart defects usually develop while a baby is in the womb. Heart defects can develop as the heart develops, about a month after conception, changing the flow of blood in the heart. Some medical conditions, medications, and genes may play a role in causing heart defects. Heart defects can also develop in adults. As you age, your heart's structure can change, causing a heart defect.
Causes of cardiomyopathy
The cause of cardiomyopathy, a thickening or enlarging of the heart muscle, may depend on the type:
- Dilated cardiomyopathy- The cause of this most common type of cardiomyopathy often is unknown. It may be caused by reduced blood flow to the heart (ischemic heart disease) resulting from damage after a heart attack, infections, toxins, and certain drugs. It may also be inherited from a parent. It usually enlarges (dilates) the left ventricle.
- Hypertrophic cardiomyopathy- This type, in which the heart muscle becomes abnormally thick, usually is inherited. It can also develop over time because of high blood pressure or aging.
- Restrictive Cardiomyopathy- This least common type of cardiomyopathy, which causes the heart muscle to become rigid and less elastic, can occur for no known reason. Or it may be caused by diseases, such as connective tissue disorders, an excessive iron buildup in your body (hemochromatosis), the buildup of abnormal proteins (amyloidosis) or by some cancer treatments.
Causes of heart infections
A heart infection, such as endocarditis, is caused when an irritant, such as a bacterium, virus or chemical, reaches your heart muscle. The most common causes of heart infection include:
- Bacteria
- Viruses
- Parasites
Causes of valvular heart disease
There are many causes of diseases of your heart valves. You may be born with valvular disease, or the valves may be damaged by conditions such as:
- Rheumatic fever
- Infections (infectious endocarditis)
- Connective tissue disorders
What are the risk factors for Cardiovascular diseases?
Risk factors for developing heart disease include:
 Age. Aging increases your risk of damaged and narrowed arteries and weakened or thickened heart muscle.
Age. Aging increases your risk of damaged and narrowed arteries and weakened or thickened heart muscle.- Sex. Men are generally at greater risk of heart disease. However, women's risk increases after menopause.
- Family history. A family history of heart disease increases your risk of coronary artery disease, especially if a parent developed it at an early age (before age 55 for a male relative, such as your brother or father, and 65 for a female relative, such as your mother or sister).
- Smoking. Nicotine constricts your blood vessels, and carbon monoxide can damage their inner lining, making them more susceptible to atherosclerosis. Heart attacks are more common in smokers than in nonsmokers.
- Certain chemotherapy drugs and radiation therapy for cancer. Some chemotherapy drugs and radiation therapies may increase the risk of cardiovascular disease.
- Poor diet. A diet that's high in fat, salt, sugar and cholesterol can contribute to the development of heart disease.
- High blood pressure. Uncontrolled high blood pressure can result in hardening and thickening of your arteries, narrowing the vessels through which blood flows.
- High blood cholesterol levels. High levels of cholesterol in your blood can increase the risk of formation of plaques and atherosclerosis.
- Diabetes. Diabetes increases your risk of heart disease. Both conditions share similar risk factors, such as obesity and high blood pressure.
- Obesity. Excess weight typically worsens other risk factors.
- Physical inactivity. Lack of exercise also is associated with many forms of heart disease and some of its other risk factors, as well.
- Stress. Unrelieved stress may damage your arteries and worsen other risk factors for heart disease.
- Poor hygiene. Not regularly washing your hands and not establishing other habits that can help prevent viral or bacterial infections can put you at risk of heart infections, especially if you already have an underlying heart condition. Poor dental health also may contribute to heart disease.
What are the Complications of Heart diseases?
The Complications of heart disease include:
 Heart failure. One of the most common complications of heart disease, heart failure occurs when your heart can't pump enough blood to meet your body's needs. Heart failure can result from many forms of heart disease, including heart defects, cardiovascular disease, valvular heart disease, heart infections or cardiomyopathy.
Heart failure. One of the most common complications of heart disease, heart failure occurs when your heart can't pump enough blood to meet your body's needs. Heart failure can result from many forms of heart disease, including heart defects, cardiovascular disease, valvular heart disease, heart infections or cardiomyopathy.- Heart attack. A blood clot blocking the blood flow through a blood vessel that feeds the heart causes a heart attack, possibly damaging or destroying a part of the heart muscle. Atherosclerosis can cause a heart attack.
- Stroke. The risk factors that lead to cardiovascular disease also can lead to an ischemic stroke, which happens when the arteries to your brain are narrowed or blocked so that too little blood reaches your brain. A stroke is a medical emergency — brain tissue begins to die within just a few minutes of a stroke.
- Aneurysm. A serious complication that can occur anywhere in your body, an aneurysm is a bulge in the wall of your artery. If an aneurysm bursts, you may face life-threatening internal bleeding.
- Peripheral artery disease. Atherosclerosis also can lead to peripheral artery disease. When you develop peripheral artery disease, your extremities — usually your legs — don't receive enough blood flow. This causes symptoms, most notably leg pain when walking (claudication).
- Sudden cardiac arrest. Sudden cardiac arrest is the sudden, unexpected loss of heart function, breathing and consciousness, often caused by an arrhythmia. Sudden cardiac arrest is a medical emergency. If not treated immediately, it is fatal, resulting in sudden cardiac death.
How can you prevent cardiovascular diseases?

Certain types of heart disease, such as heart defects, can't be prevented. However, you can help prevent many other types of heart disease by making the same lifestyle changes that can improve your heart disease, such as:
- Quit smoking
- Control other health conditions, such as high blood pressure, high cholesterol, and diabetes
- Exercise at least 30 minutes a day on most days of the week
- Eat a diet that's low in salt and saturated fat
- Maintain a healthy weight
- Reduce and manage stress
- Practice good hygiene
Keeping Cardiovascular Disease Under Control- Sometimes, developing cardiovascular disease is unavoidable—your age or family history are factors that are out of your control. But there are plenty of factors you can control, whether you’re already living with cardiovascular disease, or taking steps to prevent it.
Reduce Your Risk of Cardiovascular Disease- Some of the best ways to prevent cardiovascular disease, or to keep your symptoms under control, are to change your lifestyle habits.
Quit Smoking- A smoker’s risk of developing cardiovascular disease is two to four times greater than non-smokers. When you quit smoking, you not only improve your own health but that of your loved ones, too, by no longer exposing them to secondhand smoke that can raise their own chances of developing cardiovascular disease.
Reduce Your Cholesterol- The higher your total cholesterol, the higher your chances of developing cardiovascular disease. Choose foods low in cholesterol and saturated fat to keep your total blood cholesterol level under 200. There are also medications that can help if diet alone is not enough.
Control Your Blood Pressure- Hypertension, or high blood pressure, is the most common risk factor for cardiovascular disease. Reducing stress, eating healthy, and exercising will help keep your blood pressure in check, but there are also medications that provide extra help if you need it.
Stay Active-It can be hard to fit exercise into your schedule, but even mild to moderate amounts of physical activity can have a big impact on your heart health. Start by making exercise a part of your daily life. Go for walks regularly, do gardening, take the stairs instead of the elevator—even the smallest changes can make a difference.
Change Your Diet- You don’t need to give up all the foods you love, but making healthy changes to your diet, like choosing vitamin-rich foods low in cholesterol and fat, benefits your heart and your whole body.
Maintain a Healthy Weight- Carrying excess weight puts significant strain on your heart and can make other cardiovascular disease risk factors worse, such as diabetes. Eating right and exercising regularly can help shed extra pounds. But if diet and exercise aren’t enough, you could opt for bariatric surgery options that can help you overcome obesity.
Manage Stress-Life is often stressful—sometimes we just can’t avoid it. But consistent stress and anger can have damaging effects that could lead to heart attack and stroke. Manage stress by learning relaxation techniques or asking for help when you’re feeling overwhelmed. If you are feeling emotionally overwhelmed by stress, seek professional advice from Behavioral Health Specialists. Trained counselors can give you the help you need to cope with stress successfully.
How to Manage Cardiovascular Diseases?
Things that you and your health care professional can do for heart disease can be all over the map, from CPR to high-tech surgeries, to care-giving. Chances are that you, or someone you love, may need different types.
Different Interventions to manage heart diseases include:
CPR- Cardiopulmonary resuscitation (CPR) is one link in what the American Heart Association calls the chain of survival. Learn CPR for a loved one. You can use the Internet to find classes near you
Angioplasty and Stents- Angioplasty is a procedure that uses very little cutting to open blocked heart arteries. Stents can be put in during angioplasty.
Heart Bypass Surgery- This can treat heart disease when your coronary arteries are blocked. Your doctor may treat the problem by giving the blood a new pathway to the heart.
Valve Disease Treatment- When your heart valve disease needs attention, it can be treated by traditional surgery or by balloon valvuloplasty, which doesn't require as much cutting.
Cardioversion- For many people with heart disease, drugs alone won’t turn an arrhythmia into a normal heart rhythm. These people may need a procedure called cardio-version or electrical cardio-version.
EECP- This can help stimulate blood vessels to develop small branches, creating a natural bypass around narrowed or blocked arteries that cause chest pain.
Pacemakers- It’s a small device that sends electrical impulses to the heart muscle to keep up a suitable heart rate and rhythm. A pacemaker may also treat fainting spells (syncope), congestive heart failure, and hypertrophic cardiomyopathy.
Implantable Cardioverter Defibrillators (ICD)- An ICD, or implantable cardioverter defibrillator, can treat abnormal heart rhythms.
Lead Extraction- That’s the removal of one or more leads from inside the heart. Leads that are placed outside the heart during open heart surgery cannot be removed by this procedure.
Left Ventricular Assist Device (LVAD)- It’s a kind of mechanical heart. A surgeon would place it inside your chest. It would help the heart pump oxygen-rich blood throughout the body.
Heart Transplant- A person's diseased heart is replaced with a healthy donor's heart. A donor is a person who has died and whose family has agreed to donate their loved one's organs.
The different types of Medications to treat heart diseases include:
ACE Inhibitors- Angiotensin-converting enzyme (ACE) inhibitors are heart meds that widen or dilate, your blood vessels to raise the amount of blood your heart pumps and lower your blood pressure.
Angiotension II Receptor Blockers- These heart drugs decrease certain chemicals that narrow blood vessels. That allows blood to flow more easily through your body. These drugs also decrease chemicals that cause salt and fluid to build up in the body.
Antiarrhythmics- These drugs treat abnormal heart rhythms caused by the irregular electrical activity of your heart.
Antiplatelet Drugs- They are a group of powerful medications that prevent the formation of blood clots.
Aspirin Therapy- For more than 100 years, aspirin has been used as a pain reliever. Since the 1970s, aspirin has also been used to prevent and manage heart disease and stroke.
Beta-Blocker Therapy- Beta-blockers are one of the most widely prescribed classes of drugs to treat hypertension (high blood pressure). They are a mainstay treatment for congestive heart failure.
Calcium Channel Blocker Drugs- These relax blood vessels and increase the supply of blood and oxygen to the heart. They also reduce the heart's workload.
Clot Buster Drugs- Also called thrombolytic therapy, these are a type of heart medication given in the hospital through the veins (intravenous) to break up blood clots.
Digoxin- If you have heart disease, this is a medicine that helps an injured or weakened heart work more efficiently.
Diuretics- You may hear these called water pills. They help your body get rid of unneeded water and salt through urine. That makes it easier for your heart to pump. It also helps control your blood pressure.
Nitrates- These are meds that treat angina in people with coronary artery disease. They also help ease chest pain caused by blocked blood vessels of the heart.
Warfarin and Other Blood Thinners- These medicines help prevent clots from forming. Blood thinners treat some types of heart disease.
What's the Future of Cardiovascular Medicine?

Ongoing and future trends in treating Cardiovascular diseases include the following:
- Greater use of direct oral anticoagulants (DOACs) in atrial fibrillation (AFib) and other conditions;
- New paradigms in the management of mitral valve regurgitation (MR) in heart failure patients;
- Increased use of transcatheter aortic valve replacement (TAVR);
- A larger role for wearable and implantable devices and the data they collect; the advent of artificial intelligence (AI) in cardiovascular medicine; and
- A greater emphasis on cost and value.
Atrial Fibrillation
It's been eight years since the U.S.FDA approved the first DOAC, dabigatran. Since then, the use of dabigatran and the other DOACs, rivaroxaban, apixaban, edoxaban, and betrixaban, as the preferred anticoagulant prophylaxis for patients with AFib have risen significantly. Indeed, although the use of anticoagulation in AFib patients remains suboptimal, there is evidence that the percentage of patients prescribed anticoagulation has increased since their introduction.
Here are a few predictions:
- Greater use of DOACs over warfarin now that drug-specific reversal agents are available.
- Increased use of DOACs in other patient populations, such as those with cancer-associated venous thromboembolism (VTE).
- Increased use of DOACs, particularly rivaroxaban, among patients with atherosclerotic disease. This is a result of the COMPASS study, he says, which showed fewer cardiovascular and limb events in patients with peripheral artery disease (PAD) who received twice daily, low-dose rivaroxaban plus daily aspirin compared with aspirin alone. Similar results are anticipated from a second trial, VOYAGER PAD.
Another major story in the AFib realm for 2019 will be increased detection, possibly over detection, of rhythm abnormalities given the advent of wearable devices with built-in heart rate monitors and single-lead electrocardiograms (ECGs). This will likely raise concerns among the public about potential tachyarrhythmias. How cardiologists assess these patients and how they determine if the alarms are 'true positive' or 'false positive,' and how they will decide if anticoagulation is needed, remains a key challenge for our field. In addition, 2019 should see results from the AUGUSTUS trial, which is exploring the effects of apixaban vs. warfarin with or without aspirin in patients with AFib. This study, along with the recently completed PIONEER AF-PCI study, will help clinicians determine the safety of antithrombotic regimens for patients with concurrent AFib and coronary artery disease
The steam engine triggered the first industrial revolution; electric power the second; and electronics and digital technology the third. But it is the fourth industrial revolution, characterized by a fusion of technologies blurring the lines between the physical, digital, and biological spheres that holds the greatest potential for revolutionizing medicine. At its core is AI and machine learning. Artificial intelligence is defined as the ability of computer systems to perform tasks humans usually perform. Machine learning, while often used interchangeably with AI, is actually a subset of AI in which algorithms, mathematical models and/or computer systems are used to optimize the performance of a given task.
A recent publication in the Journal of the American College of Cardiology highlighted six broad areas in which AI will advance the cardiovascular field:
- Novel drug discovery/development- AI is increasingly being used to refine the selection of potential therapies by searching for patterns in molecular biology, structure-function, and clinical trial databases.
- Precision medicine- With AI, genetic information, environment, and lifestyle can be quickly assessed to determine who is most likely to benefit from certain interventions, he says.
- Integration of data from varied sources- AI enables data from varied sources, such as wearables, social media, the electronic health record (EHR), and the -omics, to be integrated into models that can predict the trajectory of both health and disease.
- Improved efficiency- AI can help reduce provider dissatisfaction and burnout by minimizing repetitive tasks, prioritizing EHR-based alerts or messages, improving and automating image interpretation in the catheterization or echocardiography laboratory, and presenting a "preferred" treatment plan based on the integration of varied data sources.
- Remote monitoring- AI can strain out clinically actionable data from the trillions of data bytes wearable devices collect.
- Increasing the value of delivered care- Artificial intelligence is an ideal population tool, given its ability to better predict individuals at greater or lesser risk of developing chronic diseases or related complications, tailoring preventive therapies and allocating limited resources to those most likely to benefit from them.
Patient Generated Data
The first "wearable" in cardiovascular medicine dates back to the 1800s when a watch with a second hand was used to measure heart rate. Today, however, wearables are more likely to be patient initiated, measuring everything from heart rate and rhythm to blood pressure, sleep quality and duration, and physical activity. There is some evidence that activity-tracking monitors can change behavior, although the long-term effects remain unknown. However, their accuracy varies, as does consumer acceptance of them, particularly in older people. In addition, most studies evaluate behavior change over a short period of time (a week to 10 days), leaving unanswered the question of any long-term impact, which is required for substantive prevention.
There is particular interest in the ability of wearables to affect clinical outcomes in cardiovascular disease. A major trial evaluating the potential of specialized software for the Apple Watch to detect abnormal heart rhythms is underway. The Apple Heart Study, a virtual, prospective, single-arm pragmatic study has enrolled more than 400,000 participants. The primary outcome is the proportion of participants with an irregular pulse detected by the watch who are diagnosed with AF on subsequent ambulatory ECG patch monitoring. A secondary outcome is to estimate the rate of initial contact with a healthcare provider within three months after the patient is notified of a pulse irregularity. Results may come in 2019.
Valvular Heart Disease
The results of the COAPT trial reported in 2018 should have significant implications for the field of valvular heart disease in 2019. The study, which showed that treatment with the MitraClip combined with guideline-directed medical therapy (GDMT), effectively reduced MR and was associated with marked clinical benefits. The results will encourage efforts to "fix MR" in patients with heart failure and secondary MR, he predicts. The key will be how to do this in a safe, effective and durable manner. Several questions remain, however, including how generalizable and translatable the results of COAPT will be in clinical practice.
First Therapy for a Fatal Heart Disease
Cardiac amyloidosis is a rare and fatal condition where proteins abnormally build up within the heart muscle, causing stiffening and eventually leading to heart failure. One of the major subtypes of the disease is transthyretin cardiac amyloidosis, in which a protein called transthyretin becomes misfolded — either due to genetic inheritance or aging — and accumulates in the heart. There are currently no approved treatments for transthyretin cardiac amyloidosis, and average life expectancy after diagnosis is just three to five years. Tafamidis is a novel oral medication that stabilizes the transthyretin protein, thus preventing it from unraveling and accumulating in heart tissue. Tafamidis is currently in the process of FDA approval. Shah notes that investigations of other therapies for cardiac amyloidosis are also ongoing. It is hoped that in the near future there will be multiple different treatments for this devasting disease. The study was supported by Pfizer, which manufactures tafamidis.
Investigating Device for Heart Failure
About half of all heart failures cases are classified as heart failure with preserved ejection fraction (HFpEF), a condition where the heart is pumping normally but is abnormally stiff. The syndrome is associated with significant morbidity and mortality and is increasing in prevalence. There is currently no effective treatment. One key feature of HFpEF is an increase in pressure in the left atrium during exercise. For close to a decade, Shah has been working with collaborators to develop a novel device to decompress the left atrium, which could improve both symptoms and outcomes in patients with HFpEF. The Interatrial Shunt Device (IASD) is implanted into a patient’s interatrial septum, where it creates a small opening between the left and right atria. This opening is designed to allow blood to redistribute to the right side, reducing pressure in the left.
Referenceshttps://www.healio.com/cardiology/news/online/%7B5cde3efa-5ece-44ec-ad71-c4c143291aa5%7D/what-is-cardiovascular-disease https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease https://www.mayoclinic.org/diseases-conditions/heart-disease/symptoms-causes/syc-20353118 https://www.webmd.com/heart-disease/guide/heart-disease-treatment-care https://www.thedacare.org/Health-Library-and-Conditions/cardiovascular/take-charge/Cardiovascular-Disease-Prevention-and-Management.aspx https://www.acc.org/latest-in-cardiology/articles/2018/12/10/14/42/early-release-feature-trends-in-cardiovascular-medicine-anticipated-for-2019
















Leave a Reply