“Respiratory disease” is a term that encompasses a variety of pathogenic conditions that affect respiration in living organisms. Respiration makes gas exchange possible in higher organisms. The gas exchange involves taking oxygen into the body and expelling carbon dioxide. The respiratory disease occurs in the respiratory tract, which includes the alveoli, bronchi, bronchioles, pleura, pleural cavity, trachea and the nerves and muscles of breathing. Respiratory diseases may be caused by infection, by smoking tobacco, or by breathing in secondhand tobacco smoke, radon, asbestos, or other forms of air pollution. Respiratory diseases include asthma, chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, pneumonia, and lung cancer. Also called lung disorder and pulmonary disease.
Types of Respiratory diseases:
There are three main types of respiratory disease:
- Airway Diseases
- Lung Tissue Diseases and
- Lung Circulation Diseases.
Airway diseases affect the tubes that carry oxygen and other gases into and out of the lungs. Airway diseases usually result in narrowing or blocking of the passageways. Lung tissue diseases affect the structure of lung tissue and result in scarring or inflammation of the lung tissue. This, in turn, makes breathing difficult. Lung circulation diseases occur when the blood vessels in the lungs become clotted, inflamed or scarred. These diseases affect the ability of the lungs to receive oxygen and produce carbon dioxide, and they may affect the functioning of the heart.
The common cold is an example of mild respiratory disease. More serious or life-threatening respiratory disorders include bacterial pneumonia, lung cancer, and pulmonary embolism. Other disorders include asthma, bronchiectasis, chronic obstructive pulmonary disease (COPD), influenza, obstructive sleep apnea syndrome, pulmonary hypertension, and tuberculosis. Some lung diseases may result in respiratory failure. Allergens, indoor air pollution, outdoor air pollution, and tobacco smoking are common risk factors for respiratory disorder. The respiratory disease affects millions, including 235 million people worldwide with asthma and 64 million with COPD.
Common respiratory diseases:- Asthma- Asthma is defined as a common, chronic respiratory condition that causes difficulty breathing due to inflammation of the airways. Asthma symptoms include dry cough, wheezing, chest tightness and shortness of breath.
- Chronic Obstructive Pulmonary Disease (COPD)- Chronic obstructive pulmonary disease is an umbrella term that encompasses several respiratory illnesses that cause breathlessness, or the inability to exhale normally. People usually experience symptoms, including shortness of breath, and normally cough up sputum (mucus from the lungs), especially in the morning. COPD can be tricky for some people to identify because symptoms are often mistaken for the gradual aging process and body deterioration. In fact, COPD can develop over the course of several years without any signs of shortness of breath. This disease is generally associated with cigarette smoking. It’s rare to see people with COPD who haven’t been exposed to some sort of smoking. People can experience varying severity levels of COPD. At its most severe, it can cause people difficulty doing everyday activities.
- Chronic Bronchitis- Chronic bronchitis is a form of COPD emphasized by a chronic cough. Usually, people cough up sputum (mucus from the lungs), especially in the morning. This happens because mucus glands in the airways increase output, and patients have to cough that extra secretion out. Since chronic bronchitis is a form of COPD, it’s treated the same way. People can also develop acute bronchitis, which is not a long-term disease but rather an infectious problem. It develops from a viral or bacterial infection and can be treated with antibiotics. Symptoms associated with acute bronchitis will subside once the infection has resolved.
- Emphysema- Emphysema is a serious respiratory disease, which is another form of COPD. The most common cause is smoking. Those who suffer from emphysema have trouble exhaling air from their lungs. Cigarette smoke damages the air sacs in the lungs to a point where they can no longer repair themselves. This respiratory system illness most commonly leads to respiratory failure and the need for extra oxygen to meet breathing needs. Emphysema evolves slowly over the years, and there is no cure; however, those who quit smoking are more likely to see the disease’s progression slow.
- Lung Cancer- With the ability to develop in any part of the lungs, this cancer is difficult to detect. Most often, cancer develops in the main part of the lungs near the air sacs. DNA mutations in the lungs cause irregular cells to multiply and create an uncontrolled growth of abnormal cells, or a tumor. These tumors interfere with the regular functions of the lungs. Symptoms can take years to appear but include things like chronic coughing, changes in voice, harsh breathing sounds and coughing up blood.
- Cystic Fibrosis/Bronchiectasis- Cystic fibrosis is a genetic respiratory disease caused by a defective gene that creates thick and sticky mucus that clogs up tubes and passageways. This mucus causes repeat, and dangerous, lung infections, as well as obstructions in the pancreas that prevent important enzymes from breaking down nutrients for the body. Symptoms of cystic fibrosis include salty-tasting skin, chronic coughing, frequent lung infections and a poor growth rate in children.
- Pneumonia- Pneumonia is a common lung disease caused by an infection in the air sacs in the lungs. The infections can be bacterial, viral or fungal. Most people can recover in one to three weeks, but for certain people, pneumonia can be extremely serious and even life-threatening. The very young and the very old are more at-risk for pneumonia and complications associated with pneumonia. Patients can be at increasingly susceptible to pneumonia, based on their smoking history or just their overall immune status. If they are frail or sickly, they can develop pneumonia more readily than young, healthy, well-nourished people. Symptoms, which include cough, fever, shaking chills and shortness of breath, can range from mild to severe. It’s really important for adults over 65 or those with other chronic diseases to get the pneumococcal pneumonia vaccine. Additional suggested ways to prevent this respiratory condition include washing hands frequently and getting the flu shot.
- Pleural Effusion- Pleural effusion is a collection of fluid between the lung and the chest wall in what’s called the pleural space. The fluid can collect for a variety of reasons, including pneumonia, cancer or congestive heart failure. Usually, patients notice symptoms of increasing chest discomfort and shortness of breath. Those with this diagnosis usually undergo a procedure to remove the fluid, which allows the lung to re-expand, allowing the patient to breathe better. Then, the fluid is tested to determine what’s causing it and a treatment plan is formed.
Managing respiratory diseases
Treatment can ease symptoms, prevent complications, and generally slow disease progression. Your healthcare team may include a lung specialist (pulmonologist) and physical and respiratory therapists.
specialist (pulmonologist) and physical and respiratory therapists.
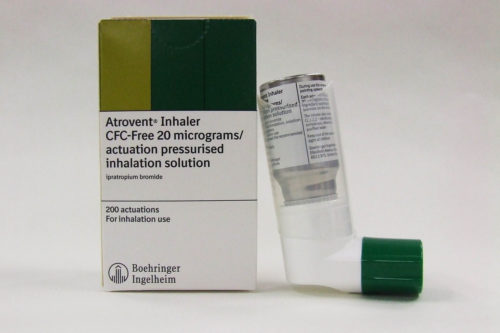
Bronchodilators are medications that help relax the muscles of the airways, widening the airways so you can breathe easier. They’re usually taken through an inhaler or a nebulizer. Glucocorticosteroids can be added to reduce inflammation in the airways. To lower risk of other respiratory infections, ask your doctor if you should get a yearly flu shot, pneumococcal vaccine, and a tetanus booster that includes protection from pertussis (whooping cough).
Oxygen therapy- If your blood oxygen level is too low, you can receive supplemental oxygen through a mask or nasal cannula to help you breathe better. A portable unit can make it easier to get around.
Surgery- Surgery is reserved for severe COPD or when other treatments have failed, which is more likely when you have a form of severe emphysema. One type of surgery is called bullectomy. During this procedure, surgeons remove large, abnormal air spaces (bullae) from the lungs. Another is lung volume reduction surgery, which removes damaged upper lung tissue. Lung transplantation is an option in some cases.
Lifestyle changes- Certain lifestyle changes may also help alleviate your symptoms or provide relief.
- If you smoke, quit. Your doctor can recommend appropriate products or support services.
- Whenever possible, avoid secondhand smoke and chemical fumes.
- Get the nutrition your body needs. Work with your doctor or dietician to create a healthy eating plan.
- Talk to your doctor about how much exercise is safe for you.
Medications- Medications can reduce symptoms and cut down on flare-ups. It may take some trial and error to find the medication and dosage that works best for you. These are some of your options:
- Inhaled bronchodilators- Medicines called bronchodilators help loosen tight muscles of your airways. They’re typically taken through an inhaler or nebulizer.
- Short-acting bronchodilators last from four to six hours. You only use them when you need them. For ongoing symptoms, there are long-acting versions you can use every day. They last about 12 hours. Some bronchodilators are selective beta-2-agonists, and others are anticholinergics. These bronchodilators work by relaxing tightened muscles of the airways, which widens your airways for better air passage. They also help your body clear mucus from the lungs. These two types of bronchodilators can be taken separately or in combination by inhaler or with a nebulizer.
- Corticosteroids- Long-acting bronchodilators are commonly combined with inhaled glucocorticosteroids. A glucocorticosteroid can reduce inflammation in the airways and lower mucus production. The long-acting bronchodilator can relax the airway muscle to help the airways stay wider. Corticosteroids are also available in pill form.
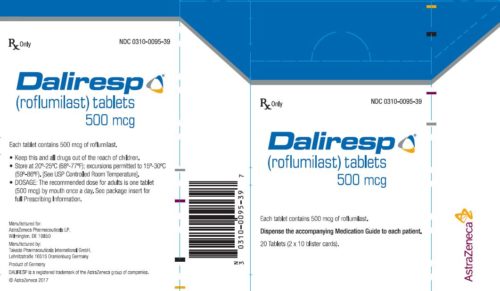
- Phosphodiesterase-4 inhibitors- This type of medication can be taken in pill form to help reduce inflammation and relax the airways. It’s generally prescribed for severe COPD with chronic bronchitis.
- Theophylline- This medication eases chest tightness and shortness of breath. It may also help prevent flare-ups. It’s available in pill form. Theophylline is an older medication that relaxes the muscle of the airways, and it may cause side effects. It’s generally not a first-line treatment for COPD therapy.
- Antibiotics and antivirals- Antibiotics or antivirals may be prescribed when you develop certain respiratory infections.
Management of respiratory diseases: What's ahead?
Researchers are working on new therapies to treat the symptoms of chronic obstructive pulmonary disease (COPD), like shortness of breath, lung inflammation, and chronic cough. Some are already available, while others are still being tested.
Valve SurgeryAs the air sacs in your lung get larger, your lung can fill with too much air every time you breathe in. In some patients with overaerated lungs, if a portion of the lung is removed, they may feel a lot better. There’s less trapping of air. Because of that, the standard treatment has been to take out the damaged part of your lung with surgery, but valve surgery is now another option. Your surgeon can use a bronchoscope to put a one-way valve in your airway. This allows the overexpanded part of your lung to release air out of the airway, but not to let air in.
Combination TherapyCOPD medications, like long-acting beta-2 agonists (LABAs) and long-acting muscarinic antagonists (LAMAs), can be used together to offer more relief of your symptoms. Both types of drugs make your airways smaller. You could start out with a LABA and add a LAMA later, but you should not hesitate to start treatment with both as a combination. You can now get combinations of all of your drugs in one inhaler, so it’s a more convenient way to deliver your medication.
Pulmonary RehabIf your COPD symptoms have affected your quality of life, led to too much weight loss, or you’ve become weak and less active, pulmonary rehabilitation may help. In pulmonary rehab, you learn how to exercise, get the right vaccinations, and get nutritional counseling. It’s not something you have to do indefinitely. It’s maybe three times a week, usually for an hour. You can work out on the machines and weights with a trainer. A lot of people with COPD really benefit from these programs.
IL-5 drugsDoctors can use blood tests to divide people with COPD into smaller groups to prescribe more targeted treatments for them. For example, one group includes people with eosinophilia, a high number or percentage of white blood cells called eosinophils in their blood. Eosinophilia is more common in asthma, but some people with COPD have a high amount of these white blood cells, too. If your levels are above 300, a new group of biologic drugs called IL-5 antagonists might work well for you.
Stem Cell TherapyEmphysema is one of the major health problems involved in COPD. Over many years, your lungs become damaged and diseased. Sacs inside them called alveoli grow too large. Their tissue breaks down, and that causes severe shortness of breath. The idea behind this therapy is that you take stem cells and use them to create new alveolar cells. It’s going to become a reality for treating COPD, but we’re not there yet.
New Class of Kinase Inhibitors Are Potential COPD Anti-inflammatory Therapies
Inhaled corticosteroids are commonly used as an anti-inflammatory treatment for COPD. Combined with bronchodilators (which open the airways of the lungs), they were shown to improve lung function, reduce disease progression, and increase the quality of life, compared to single therapy. NSKIs are a new class of kinase inhibitors that suppress specific protein kinase families at the same time. Researchers have evaluated the effectiveness of RV1088 and RV568 (identified by RespiVert) to suppress inflammatory cytokines in airway cells taken from COPD patients. The results were compared with the effects of a conventional corticosteroid and of three single kinase inhibitors — doramapimod, Sprycel, and R343. Both NSKIs were found to be more effective in suppressing the production of inflammatory cytokines than the other therapies. Their study has demonstrated that NSKIs are promising candidates for the development of urgently required anti-inflammatory COPD therapies. They believe that these preclinical findings introduce RV1088 and RV568 as promising new therapies for COPD. These compounds are currently being developed in a clinical program to be tested in patients in future clinical trials.
The Future of Lung Cancer Care Is CombinationsImmunotherapy revolutionized the way we treat cancer. And now, researchers are using drugs to help jumpstart the immune system alongside chemotherapy to keep treatment moving forward. Cutting-edge clinical trials are monitoring how well these combinations work in patients with non-small cell lung cancer. In one of the features, these trials are discussed in more depth — the agents used, which protein or mutation they target, and, most important, how patients are faring. So far, researchers have seen positive results, and they are learning more about toxicities that can plague patients. One of those patients shares her journey with stage 4 disease that spread to her lymph nodes, bones, and vertebrae. Finding the last spot in a combination immunotherapy clinical trial that was testing investigational therapies, she took a chance, despite her fears, and qualified.
Breakthrough discovery will change treatment for COPD patients
Permanent lung damage caused by chronic obstructive pulmonary disease (COPD) starts much earlier than previously thought, even before patients are showing symptoms. These are the findings of a new study recently published in The Lancet Respiratory Medicine. The breakthrough discovery, led by Dr. Tillie-Louise Hackett, associate professor in the University of British Columbia's faculty of medicine, will dramatically change how patients are treated for COPD, the leading cause of hospital admissions in B.C. and Canada. The new findings also suggest previous large clinical trials testing new COPD treatments may have failed because patients already had substantial lung damage. If the same drugs were tested on patients with more mild forms of the disease, and less tissue damage, the results could be very different.
A new way to target lung cancer could be on the horizon
A key molecular player has been identified by scientists in a sub-type of lung cancer which could lead to a new way to tackle the disease. Based at the University of Cambridge, UK, Cancer Research funded scientists have discovered lung squamous cell carcinoma (LUSC) cells containing high amounts of a protein called BCL11A. This discovery has the potential of finding a new way to treat lung cancer. The study showed that manipulating the gene responsible for the protein stopped the development of LUSC in a mouse model of lung cancer disease. The study also revealed a signaling pathway that BCL11A was involved in, as well as a potentially druggable target, called SETD8. Targeting this molecule both genetically and with early forms of drugs, selectively targeted LUSC cancer cells growing in the lab. These breakthrough discoveries have led to further funding being granted by Cancer Research UK to facilitate the development of a drug to target the protein, which could one day lead to a new treatment option for some people with lung cancer.
Source Referenceshttps://www.cancer.gov/publications/dictionaries/cancer-terms/def/respiratory-disease https://www.healio.com/infectious-disease/news/online/%7Bebb671bb-8ff7-47d7-a735-c34f266e6f71%7D/what-are-respiratory-disorders https://www.unitypoint.org/homecare/article.aspx?id=2448b930-1451-43e4-8634-c0c16707c749 https://medlineplus.gov/ency/article/000066.htm https://www.curetoday.com/publications/cure/2018/2018-lung-1/the-future-of-lung-cancer-care-is-combinations https://medicalxpress.com/news/2018-07-breakthrough-discovery-treatment-copd-patients.html https://www.webmd.com/lung/copd/features/copd-new-treatments#1















Leave a Reply