Healthcare Management mainly involves management of a Healthcare System, Service or a facility which may involve a clinic, hospital and any other healthcare facilities. A healthcare manager is responsible for smooth functioning of the service or a facility.
Healthcare Management vs. Healthcare Administration
 Healthcare administration and healthcare management are often incorrectly viewed as the same fields. While there are similarities, there are also unique differences between the two career focuses.
The primary difference between healthcare management and healthcare administration
Healthcare management focuses on overseeing the direction of a healthcare facility or system, organization-wide initiatives, and “big picture” needs, while healthcare administration focuses on individual departments and budgets, day-to-day operations, and staffing.
Healthcare management also focuses on the overall needs of the entire organization. By comparison, healthcare administration is more focused on individual areas and departments. A healthcare manager helps direct organizational policies and procedures and shares that information with the entire system, while a healthcare administrator is more focused on best using and directing his or her staff within a department.
Healthcare administration and healthcare management are often incorrectly viewed as the same fields. While there are similarities, there are also unique differences between the two career focuses.
The primary difference between healthcare management and healthcare administration
Healthcare management focuses on overseeing the direction of a healthcare facility or system, organization-wide initiatives, and “big picture” needs, while healthcare administration focuses on individual departments and budgets, day-to-day operations, and staffing.
Healthcare management also focuses on the overall needs of the entire organization. By comparison, healthcare administration is more focused on individual areas and departments. A healthcare manager helps direct organizational policies and procedures and shares that information with the entire system, while a healthcare administrator is more focused on best using and directing his or her staff within a department.
Healthcare management job titles may include:
- Hospital administrator
- Executive director
- Practice administrator
- Public health director
- Health advocate
- Social welfare administrator
Healthcare administration job titles may include:
- Clinic director
- Hospice care director
- Health services manager
- Practice administrator
- Medical records manager
- Practice or office manager
Benefits of Healthcare Management
Health care is one of the fastest-growing industries in the world. All health care systems, whether public or private, face the challenge of sustainability. Costs have risen due to demographic changes (e.g. an ageing population, the increase in non-communicable diseases, but also the ongoing HIV/AIDS challenge in Sub-Saharan Africa) as well as technological developments to meet the expectations and needs of the patient population. The recent economic challenges and the Covid-19 pandemic have increased the challenge the health care industry is facing. Maintaining funding levels that are appropriate to the technology innovation curve, the demographic-epidemiological curve, and citizen expectations is an unprecedented challenge for nearly all health systems
Critical Components of Healthcare Management
Administration, finance, supply management, human resources management, etc.
High hospital performance relies on professional management assured by competent teams covering a wide skillset. Scope and content of hospital management, financial management and different administrative functions are context and country specific and will differ depending on ownership, autonomy levels, provider payment mechanisms etc.
Workload Indicators of Staffing Need (WISN) provides health managers a systematic way to make staffing decisions in order to manage their valuable human resources well.
Quality and Safety Management
High quality hospital services are safe, effective and people-centred. Tied with this, health services should be timely, equitable, integrated and efficient. Hospitals reorganize processes and reorient their logistical efforts to make care accessible, acceptable and continuous from the patient’s point of view. High quality care also means that people are informed and empowered to take decisions regarding their health care.
Improving the quality of services delivered in hospitals has potential to improve the performance of hospitals and increase demand of services by users, as well as improve the overall trust that patients have in health institutions.
Quality of care is dependent on three inter-linked factors:
- Structural inputs: investments in health facility infrastructure such as water sanitation and hygiene or human resources.
- Process measures: what and how care is delivered according to evidence-based guidelines such as infection prevention and control.
- Outcomes: health status of the patient/population.
Quality strategies and approaches:
- National Quality Policy and Strategies The development, refinement and implementation of a national quality policy and strategy (NQPS) is an emerging priority for countries as they strive to systematically improve the performance of their health care systems. The NQPS handbook includes several references to hospitals and lists hospitals as stakeholders. Key quality tools and resources directly relevant to hospitals are placed on the NQPS webpage.
Safety tools and programmes:
- Patient Safety: Making health care safer This brochure illustrates the importance of safe care for everyone, what the burden and impact of unsafe care is, and WHO’s approach to tackling the issue of unsafe care. The brochure also contains a comprehensive collation of key WHO materials and activities in to generate improvements at the front line.
- Patient friendly hospital initiative assessment standards This mechanism provides institutions with a means to determine the level of patient safety.
- WHO's Global Patient Safety Challenge: Medication Without Harm This brochure outlines the vision and strategic direction of this global initiative aiming to reduce the level of severe, avoidable harm related to medications by 50% over the next five years, globally.
- Minimal Information Model for Patient Safety (MIMPS) MIMPS has been developed to provide a simple tool to start collecting data on patient safety incidents to assist in data analysis and extract the minimal, but necessary information to learn from incidents in order to avoid recurrence of same types of incidents in the future.
- SAVE LIVES: Clean Your Hands This annual campaign aims to progress the goal of maintaining a global profile on the importance of hand hygiene in health care and to ‘bring people together’ in support of hand hygiene improvement globally.
Hand Hygiene in Health Care
This WHO guidelines provide health-care workers (HCWs), hospital administrators and health authorities with a thorough review of evidence on hand hygiene in health care and specific recommendations to improve practices and reduce transmission of pathogenic microorganisms to patients and HCWs. It contains a range of tools.
- Hand Hygiene Self-Assessment Framework pdf, 469kb This framework is a systematic tool with which to obtain a situation analysis of hand hygiene promotion and practices within an individual health-care facility.
- Injection safety tools and resources This website contains a range of resources valuable to hospital managers.
- Guidelines on core components of infection prevention and control programmes at the national and acute health care facility level These guidelines cover eight areas of IPC and comprise 14 recommendations and best practice statements, ranging from the need to set up national IPC programmes, through to a focus on workload, staffing, bed occupancy and WASH.
Capacity building of hospital managers
Professional hospital management requires wide range of competencies which get acquired through training and experience.
The International Hospital Federation developed a global healthcare management competency framework based on five key domains:
- Leadership
- Communication and Relationship Management
- Professional and Social Responsibility
- Health and Healthcare Environment and
- Business
It specifies 27 sub-domains and 87 competencies. Establishing a national or institutional hospital management competencies matrix constitutes an initial step for the development of a comprehensive capacity building program.
Different countries and regions have a wide range of training institutions or training initiatives offering different modes of learning: bachelors and masters courses, e-learning, short courses, workshops, custom-made trainings, competency-based modular delivery of a large variety of topics, linking course work with field practice & mentorship for greater effectiveness, capacity building project (blended learning), and community of practices.
Healthcare Management - Future Trends
 Advancements in technology have changed the way consumers manage their own healthcare and interact with medical providers. A recent survey from Morning Consult found that 34% of U.S. adults currently track or manage their health using a mobile app. Specialized care delivery facilities are on the rise, and new tech trends are making healthcare more personalized than ever. In addition, telehealth technology allows patients to access health services, such as virtual appointments, from the comfort of their homes.
Advancements in technology have changed the way consumers manage their own healthcare and interact with medical providers. A recent survey from Morning Consult found that 34% of U.S. adults currently track or manage their health using a mobile app. Specialized care delivery facilities are on the rise, and new tech trends are making healthcare more personalized than ever. In addition, telehealth technology allows patients to access health services, such as virtual appointments, from the comfort of their homes.
Providing a stellar patient experience is top priority in the healthcare industry, and many providers are shifting their focus from volume- to value-based care. Instead of following a traditional fee-for-service model, value-based care rewards providers by determining the cost of the service as it relates to the quality of care, patient outcomes, and other factors. Forbes predicts that up to 15% of global healthcare spending will be on value-based care by the end of 2019. As technology improves, allowing medical professionals to better track quality of care, bundle packages, and transition to Electronic Health Records (EHRs), value-based care will become a more viable option.
The future of healthcare services will ask professionals to integrate traditional skills in care, communication, and leadership with new skills in technology and analytics. These new skills will work in tandem with the adoption of the following trends and advancements:
Specialized Outpatient Care Centers
To improve the patient experience, healthcare providers are offering more timely and specialized treatment. Outpatient surgeries, or same-day surgeries, are typically less complex, and they include cataract removals and colonoscopies. Instead of the traditional hospital setting, these procedures are now offered at ambulatory surgery centers (ASCs).
ASCs and other specialized outpatient care centers help reduce overall medical costs by moving specialized services to locations with that sole focus. This frees up space and staff at larger medical institutions, while also providing more focused care for the patient at the ASC. The quality of care is also improved, as specialists are able to work in an environment focused around their area of expertise. ASCs also require reporting and quality measures almost double those of outpatient surgeries in similar hospital settings.
Healthcare professionals must educate consumers on the benefits of these specialized facilities through the use of quality data that compares ASCs and hospitals for outpatient care. Health educators play an important role in helping raise awareness about ASCs to the public and can help navigate patients to an ASC environment as appropriate.
Precision Medicine for Personalized Healthcare
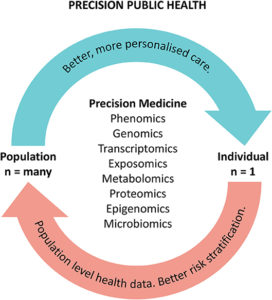 In contrast to a one-size-fits-all approach, precision medicine takes into account an individual’s genes, environment, and lifestyle to identify personalized disease treatments and prevention strategies. Best known for its uses in oncology, such as tracking the genetic profile of patient’s tumor cells to identify the most effective forms of treatments, precision medicine is also impacting pharmaceutical research and healthcare technology.
In contrast to a one-size-fits-all approach, precision medicine takes into account an individual’s genes, environment, and lifestyle to identify personalized disease treatments and prevention strategies. Best known for its uses in oncology, such as tracking the genetic profile of patient’s tumor cells to identify the most effective forms of treatments, precision medicine is also impacting pharmaceutical research and healthcare technology.
With more than 6,000 known genetic diseases, healthcare organizations need the right technology to manage patient data and apply insights to patient care. According to a study by Scipher Medicine, 65% of patients prescribed the top five selling drugs in the world did not respond to treatment. However, precision medicine offers an opportunity to more accurately predict if a patient will respond to a particular drug therapy, helping to lower healthcare costs associated with wasted prescriptions and ineffective patient treatment, as well as to prevent unnecessary side effects and drug interactions.
Precision medicine is also expanding to the realm of preventive healthcare, allowing patients to make lifestyle choices to stay healthy and track their physical well-being. As the future of healthcare technology gains a more patient-centered focus, healthcare professionals will utilize existing technologies like wearables to collect consumer health data and analyze it in a way that patients can understand and leverage with ease.
Predictive Analytics for Population Health Management
 Many facets of the healthcare industry are relying on data more each year. The information gathered allows healthcare providers to leverage analytics to improve the health of the population and identify at-risk individuals through population health management (PHM).
Many facets of the healthcare industry are relying on data more each year. The information gathered allows healthcare providers to leverage analytics to improve the health of the population and identify at-risk individuals through population health management (PHM).
PHM is the aggregation of patient data across multiple sources, including payers, hospitals, primary care providers, specialists, pharmacies, and more. The analysis of this data to create a single patient record helps healthcare providers to improve both clinical and financial outcomes. Forbes predicts that 50% of all healthcare companies will have dedicated resources to access, share, and analyze real-world data to use across their organizations by the end of 2019.
Healthcare administrative professionals and data scientists receive this data in real-time and use the insights gained from its analysis to identify and address gaps in patient care within the population. They can use this information to develop care management programs that optimize outcome and cost savings. The future of healthcare services requires intelligent application of PHM programs by healthcare administrators, who can create and implement policies, plan and oversee budgets, and ensure compliance with procedures and regulations.
Real-time Data Visualization
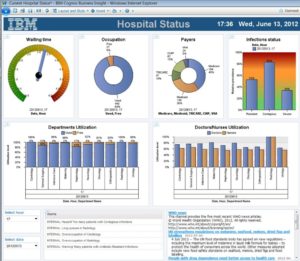 The use of big data in the medical field is not a new phenomenon, and the future of healthcare includes advances in predictive analytics to increase response efficiency, provide real-time reporting, and identify at-risk populations. Predictive analytics is on track to be a more than $9 billion industry by 2020. It works by using historical information and transactional data to predict health-related occurrences, such as how the weather might affect patients with respiratory ailments.
The use of big data in the medical field is not a new phenomenon, and the future of healthcare includes advances in predictive analytics to increase response efficiency, provide real-time reporting, and identify at-risk populations. Predictive analytics is on track to be a more than $9 billion industry by 2020. It works by using historical information and transactional data to predict health-related occurrences, such as how the weather might affect patients with respiratory ailments.
As healthcare organizations move toward sharing more data with each other, the collection and creation of larger datasets will increase accuracy and allow organizations to spot trends. For example, a network of hospitals that shares data can better predict when flu season will hit and how severe the strain will be.
Healthcare administrators must keep up with ever-evolving technologies to prepare organizations to move toward real-time data visualization to meet patient demands. Administrators must collaborate with doctors, technicians, medical centers, IT teams, and government bodies to facilitate the implementation of advanced technologies.
Telehealth
 Advancements in the future of healthcare will also have an impact on the treatment of a variety of medical needs. Telehealth — the ability to engage in healthcare quickly and seamlessly through technology like smartphones, laptops, and streaming services — marks a significant shift in the modern world of healthcare. Accessibility is improved, as those who do not live near a medical facility can leverage telehealth to connect with their healthcare professional more regularly. Additionally, those who require treatment for certain disorders, such as a communication disorder or a mental health disorder, can engage in treatment from the comfort of their home, via video chat.
Advancements in the future of healthcare will also have an impact on the treatment of a variety of medical needs. Telehealth — the ability to engage in healthcare quickly and seamlessly through technology like smartphones, laptops, and streaming services — marks a significant shift in the modern world of healthcare. Accessibility is improved, as those who do not live near a medical facility can leverage telehealth to connect with their healthcare professional more regularly. Additionally, those who require treatment for certain disorders, such as a communication disorder or a mental health disorder, can engage in treatment from the comfort of their home, via video chat.
The application of telehealth to communication disorders is still relatively new, but degree programs in communication sciences and disorders are preparing aspiring speech language pathologists and other professionals for the intermingling of traditional methods of care and telehealth.
Improving Patient Experience
Patient wellness is the heart of healthcare. As technologies advance and the prevalence of data grows, healthcare professionals use insights from the latest trends to help improve the quality of patient care. A career in the healthcare industry can be rewarding, as medical professionals play a hand in improving population health, as well as helping to lower healthcare costs.

















Leave a Reply